Questions about the birth and the time after: What you should know
From week to week, not only the belly grows, but also the birth date is getting closer. With each change of weeks, expectant parents face different tasks and decisions, and new questions arise. Do you feel the same way? Then you will find helpful information on the topic of birth and the time afterwards in this article. In addition, mom Christina reports on her experiences and answers some questions about the particularities of giving birth during a pandemic.
Preparation for birth
Birth preparation course: Do I have to take one and what should I look out for?
Even before the actual birth begins, the topic plays a major role for pregnant women. For example, many attend a childbirth preparation course to prepare their body and psyche for the birth and to exchange ideas with other pregnant women. Childbirth preparation courses are by no means compulsory, but can be very useful. They offer pregnant women the opportunity to familiarize themselves with the situation and eliminate possible fears or worries. In the courses, not only breathing, body and relaxation exercises for pregnancy and birth are learned, but also questions of the pregnant women are specifically answered. In addition, the processes of pregnancy and birth are explained and possible complications are also discussed. Pregnant women can also try out their first birth positions in these courses and thus get a feeling for what feels right for them. Other topics that can be discussed in childbirth preparation courses include painkillers, baby care, breastfeeding or the process of a C-section. Such courses can also be a great opportunity for your partner to participate more intensively in the pregnancy and to learn how to be supportive during birth. If you decide to take a childbirth preparation course, you should look for a place around the 18th week of pregnancy. However, the ideal time to start the course is rather towards the end of pregnancy, more precisely, towards the end of the second trimester. At this point you have already gained experience in pregnancy and can feel your baby, but the birth is not yet imminent.

Tip: You should start looking for a midwife as soon as the test is positive!
Clinic and birth registration: Where should the birth of my child take place?
Some organizational matters also need to be clarified in relation to the birth. The first thing to decide is where the birth should take place: in a clinic, a birth center or even at home? In a clinic, the expectant mamas are in an unfamiliar environment and have no permanent midwife, unless you take care of a midwife on call beforehand, who will attend to the birth. The advantage of giving birth in a hospital is the monitoring options and the option to receive strong pain medication. In case of emergencies, it is easier to be treated in a hospital than in a birth outside a hospital. If you wish to give birth outside a hospital, you should discuss this with your doctor and midwife. After all, in addition to the needs of the pregnant woman, the health of the baby is of course the top priority. When giving birth in a birth center, pregnant women have contact with the midwife team beforehand and their midwife is on call. However, only the administration of mild painkillers is possible there. The same applies to a home birth. Here, the baby is born in a familiar environment and the expectant mother is accompanied by her midwife the entire time. In birth centers and in a home birth, the atmosphere is more intimate and the contact with the midwives is usually more familiar, since you have a permanent midwife. In a high-risk pregnancy, delivery in a birth center or at home is not possible. This is because it is not possible to act in emergencies because the appropriate means and possibilities for treatment are not available.
Once this decision is made, the next decision is already at hand. In the event that the birth is to take place in a clinic, the question now arises, in which clinic. This decision does not have to be made right at the beginning of pregnancy, but should be decided around the 30th week of pregnancy. Important criteria for the selection are, among others, the health condition of mother and baby and the mother’s need for safety. If the pregnancy goes smoothly and mother and baby are healthy, it is the woman’s free choice where to deliver. What matters here is where the expectant mom feels safe. In a clinic with or without a premature baby ward, a clinic with small delivery rooms or, for example, a university clinic. If the decision is made in favor of a birth center or a home birth, a midwife or a midwife team should be sought from the time of the positive test.

Tip: It varies from which week of pregnancy you can register for birth at clinics. It is best to call the maternity ward in advance and make an appointment for registration. During the phone call, you can also ask what documents you need to bring with you to register for the birth.
The types of birth and positions: How should my child be born?
You may have already thought about how you want to deliver your baby. The most popular birth methods and positions include supine birth, upright birth and water birth – all three have their own advantages.
1. Birth in supine position
Delivering the baby in the supine position is the classic birthing position. Even today, most women give birth in this way. Although this birthing position is convenient for midwives and doctors, it offers few advantages for the woman. In this position, the expectant mom cannot benefit from gravity, which is why the birth costs more strength. The baby also has less space in the pelvis and there may be more pain than in other birth positions.
2. Birth in an upright position
If the birth is to take place in an upright position, pregnant women again have several options from which to choose. For example, the baby can be delivered in a kneeling or squatting position. In this position, the pelvic outlet is widened to the maximum, which can make the birth easier. At the same time, however, this position is stressful for the mother-to-be’s back and knees. To reduce the strain, you can cushion with mats or pillows and have your partner provide additional support. When giving birth in an upright position, the partner can generally support the woman very well. In addition, there are also the positions of sitting, standing or even the quadruped position. Here, various aids can be used for support, such as a birthing chair, a birthing stool or a sitting ball. The upright position has the advantage that gravity “helps” and facilitates the birth. Many pregnant women also find it easier to breathe in the various upright positions.
3. Water birth
Water birth is becoming more and more popular. Today, about every 20th child is born in a birthing tub. For this, the expectant mom lies in a tub of warm water, which helps with relaxation and can relieve pain. In addition, there is also a lower risk of perineal tear during water birth, because the muscles are more elastic. A water birth is also gentler for the newborn because he or she slides from the amniotic fluid directly into the warm water of the tub, allowing him or her to acclimate more slowly to the new environment. It is important to note that a water birth is only an option if there are no risks to the mother or baby. In case of multiple births, a bad CTG of the baby or a breech position of the baby, a water birth is not possible. If you decide to have a water birth, it is important to keep the following point in mind during preparation: For a water birth, it is important for the safety of the clinic staff that the results of an HIV test and a hepatitis C test of the pregnant woman are available. For this purpose, you can have a doctor examine you beforehand and take a blood sample.
Optimally prepare for a birth with an epidural: What should I consider before the birth?
Are you still not sure if you want to give birth with an epidural? An epidural is used as a pain inhibitor during childbirth. It involves injecting an anesthetic into the peridural space in the pregnant woman’s spine to relieve her pain. To keep all your options open for the birth, there are a few things you should keep in mind. If you are thinking about an epidural from the beginning, you can also prepare for it. The best thing to do is to ask the clinic staff when you register for the birth, so that you can be given the epidural sheet directly on the spot. Alternatively, you can call the delivery room and ask if the epidural form can be sent to you. This gives you the opportunity to fill out the form at home and bring it with you on the day of the birth.

Important: You can of course also fill out the PDA form on site if you come to the clinic for the birth and decide to have an epidural there.
HypnoBirthing: What can I do for a painless birth?
Hypnobirthing is a method of birth preparation developed in the 80s by Marie Mongan, which helps women to get into a state of relaxation and deep concentration during childbirth. In a natural birth process, there is no extreme pain and contractions. However, pain can result from pregnant women becoming tense with anxiety and increased release of stress hormones. Anxiety can therefore affect the physical process of childbirth. This is where hypnobirthing comes in and releases these fears and tension to allow the birth to proceed naturally. Through a certain type of hypnosis, the pregnant woman can relax while being fully conscious. Because of this relaxation and confidence during birth, pain and complications decrease as the body releases endorphins (“happy hormones”). These hormones lead to a feeling of well-being and counteract pain. Births can be easier and faster with this method, as pregnant women control and use their strength better. The four basic hypnobirthing techniques include breathing, visualization, relaxation and deepening. These methods of hypnobirthing can be learned in special courses. The goal of these courses is to accept one’s fears and insecurities and transform them into self-confidence. Negative assumptions should thus become positive beliefs of one’s own strength.
Packing a clinic bag: What do I need at birth?
The birth date seems almost within reach and the nest-building drive is already in full swing? Now, at the latest, many pregnant women start thinking about what should be packed in the hospital bag and what is needed for the birth. Depending on the type of birth, the clinic bag must of course be packed differently. For an outpatient birth, for example, less change of clothes is necessary because the stay in the clinic is much shorter. In general, however, you should make sure to pack comfortable clothes that don’t pinch anywhere and that you feel comfortable in. Warm socks should also not be missing from your hospital bag. Cold feet can inhibit labor during birth. You can also pack towels, washcloths, hair ties and your toiletries. For the time after the birth and the first breastfeeding attempts, it helps to have a nursing bra, nursing pads and a nipple ointment with you. Diapers and panty liners are usually provided by the hospital, but it doesn’t hurt to bring your own as a precaution. It also doesn’t hurt to bring a podusche for the postpartum flow. If you are having a water birth, you can pack bath additive and your bathrobe. A massage oil for relaxation can also be helpful during a long birth. Here, for example, the pregnancy care oil from sanosan is suitable. To feel more comfortable in the delivery room or birth center, you can also bring music or a pleasant scent that you already know. In addition, the relevant documents on the day of birth should not be missing. This includes, for example, your maternity passport, your identity card, your health insurance card and your birth certificate. If you are married, you will also need your marriage certificate. For the way home from the hospital you need baby clothes and comfortable clothes for yourself.
Do I need a separate bag for the delivery room?
For some pregnant women, the birth happens so quickly that they don’t have time to use all the things they brought with them. Others, on the other hand, are glad for everything they have packed. To be prepared for all eventualities, it makes sense to pack an extra bag for the delivery room. This way, you have all the things you need for the birth right at hand, and the person accompanying you doesn’t have to keep leaving the room because something is still missing. In this bag should be all important documents, your warm socks and the clothes you want to wear at the birth. A hair tie and lip balm should not be missing here. Many pregnant women are bothered by the hair during birth and the lips can dry out quickly due to the many deep breaths. You can also pack a few snacks in case the birth takes longer and you or your partner need some comfort food.

Induction of labor: what happens if I am past the calculated due date?
If the due date has passed, it does not mean that the birth must be induced. First, the due date is recalculated and the pregnant woman and the baby are examined every two to three days. For example, the baby’s heartbeat is checked and the amount of amniotic fluid is determined. Until the end of the 39th week of gestation, the doctor will not usually induce labor, provided there are no risks to the mother and baby. From 40 to 41 weeks, birth may be induced if it is necessary and there are risks. In the 42 SSW, the pregnancy can be induced even if there are no signs of risks. If the birth is finally induced, the expectant mom must be admitted to the hospital as an inpatient, as induction of labor can take several days. Induction of labor can be done in several ways.
1. Natural induction of labor
There are many methods to induce labor naturally. For example, labor can be induced by taking a walk and moving around. It is important here that pregnant women do not move too far from home on their own. But spicy food, an enema or even a labor cocktail with castor oil can also induce labor. Before you try to induce labor with any of these methods, you should get enough information. It is best to talk to your midwife to clarify any questions you may have and to discuss how to proceed.
2. Induction of labor with medication
If the birth is induced with medication, prostaglandins are given first. These cause the cervix to soften and open. Prostaglandins can be given in the form of tablets or as a gel for the cervix. Another option is the hormone oxytocin, which promotes contractions and induces labor.
3. Mechanical induction of labor
In mechanical induction of labor, a balloon catheter is inserted into the pregnant woman and filled with saline. This balloon exerts pressure with the filling causes a slight dilation of the cervix. The body reacts to this dilation by releasing prostaglandins. In addition, cervical massages are used to promote opening. Another method is egg release, in which the midwife carefully attempts to detach the outer covering of the amniotic sac from the cervix. The body reacts to this mechanical intervention by releasing prostaglandins.

Important: Don’t worry if your baby is waiting. You will be regularly examined by doctors and cared for by your midwife. Soon you will be holding your little miracle in your arms!
The birth
The birth begins: When do I have to go to the clinic?
The birth is probably a very exciting time for every pregnant woman, because it is clear: Soon you will hold your baby, which you have carried for so long, in your arms. However, it is not possible to make a general statement about when is the right time to go to the clinic, because every pregnant woman and every birth is different. As soon as the contractions occur every five minutes over a period of one hour and last for at least one minute, you can make your way to the clinic. If you feel comfortable at home, you can stay longer. The important thing is that you feel safe. As soon as you become unsure, you should go to the clinic, where you will be cared for by midwives and doctors.
The position of the baby at birth: what do I do if the baby is wrong side up?
Babies are naturally born with their heads down. This position of the baby is called the cranial position. However, not all babies lie head down just before birth. If the baby lies with the head in the womb and the feet and buttocks down, this is called the breech presentation. Here we distinguish different types such as the perfect foot position, in which the baby’s feet would be born first. Another position of the breech presentation is the perfect breech-foot position. In this position, the baby’s legs are crouched. The most common variant is the so-called pure breech position, in which the baby has the little feet in front of the face. In the pure breech position, a cesarean section is not necessary, but like the other positions of the breech presentation, it also offers certain risks for the baby. It is best to get information from a clinic near you that has a lot of experience with this and talk to your midwife. Every situation is different and your midwives and doctors can help you individually and answer your questions.
Painkillers: what are the drug and non-drug options?
In the early stages of birth, when the contractions are not yet very strong, a warm cherry pit pillow, for example, can help. The pillow can be placed in the area of the lower back or simply in the place where it feels good for the expectant mom. A relaxing massage or a relaxing bath in the tub can also help make the pain more bearable. It’s best to ask the midwife if this option is available and if a tub is free. Many clinics also offer acupuncture and homeopathy. Here, too, it is worth asking in advance what is possible in the respective clinic. If the pain becomes more intense as the birth progresses, you can slowly switch to painkillers. At first, mild painkillers can be administered in the form of suppositories, which initially work well for several hours. If the pain is more severe, pregnant women are given an IV line through which painkillers can be administered as an infusion. You can learn which painkillers you can take and when in a childbirth preparation course or you can discuss this individually with your midwife and your doctors.
Spontaneous cesarean section: What happens if a spontaneous cesarean section does occur during delivery?
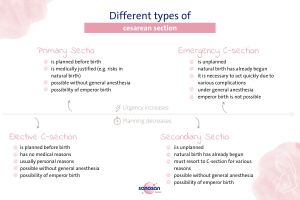
Cesarean section is a surgical procedure in which the baby is delivered by doctors. An incision is made in the lower abdomen, which is later sutured shut. There are several forms of cesarean section, each differing in urgency and planning. On the one hand, there is primary and secondary cesarean section, on the other hand, elective cesarean section and emergency cesarean section. In the case of primary cesarean section, it is already clear before the birth that the child will be delivered by cesarean section. The intervention is always planned and medically justified, for example by possible risks for mother and child. The elective C-section is performed – as the name suggests – at the request of the expectant mother. The planning of the elective cesarean section is not medically justified, but usually due to personal reasons.
Secondary cesarean section refers to a cesarean section that occurs spontaneously during childbirth. This means it was not planned beforehand and the natural birth has already started. Why it has a Secondary Sectio can have different reasons. In contrast, emergency cesarean section, emergency cesarean section differs mainly by its urgency. Like secondary cesarean section, it is not planned and it is necessary to switch to cesarean section due to complications during natural birth. The difference here is the extent of complications, which requires quick action to protect both mother and child. In this case, the operation takes place under general anesthesia, because it works faster and the child must be born within six minutes. However, emergency cesarean sections are extremely rare, and usually the procedure can be performed as a secondary cesarean section.
If the cesarean section is planned, it can usually be performed while the mother is conscious (i.e., without general anesthesia), allowing her to witness the first minutes of her newly born child. For this purpose, pregnant women are usually anesthetized with spinal anesthesia or epidural anesthesia (PDA). During the procedure, your partner sits by your head the entire time to support you. Your midwife also accompanies you and can explain what is being done and answer any questions you may have. Once your baby is born, he or she will be placed on your chest for bonding in the first few minutes, just like a natural baby. If you have any concerns or fears about a C-section, it is best to ask your midwife or a doctor if they can answer your questions.

Tip: In the case of an elective cesarean section or Primary and Secondary Sectio, there is the possibility of an emperor birth. Here, the cloth stretched between the mother’s head and abdomen is lowered when the baby is brought into the world. The light is dimmed and the baby is brought out of the womb first with the head and then with the body, as in natural birth. This gives parents the opportunity to see their child immediately and watch the birth. However, not every hospital offers an emperor birth. Therefore, it is best to ask beforehand whether this is possible.
The stages of birth: what happens during birth?

The birth begins with the opening phase. The opening phase is the period from the first contractions to the complete opening of the cervix. It is usually the longest part of the birth and lasts between six to twelve hours. Initially, contractions in this phase occur at longer intervals of about 15 minutes. As time progresses and birth occurs, the intervals then shorten to every one to two minutes.
Once the cervix is fully open (about ten centimeters), the second phase of birth begins: the exit phase. This phase is characterized by strong contractions and usually lasts between one hour and 20 minutes, but can go up to three hours. During the exit phase, there is an urge to push, which is triggered by the pressure on the cervix. If this pressing urge occurs in combination with contractions, these are called pushing contractions. Active pushing causes the baby to slide deeper into the birth canal. The contractions here occur approximately every two to four minutes and can last between 60 and 90 seconds. The exit phase of labor ends when the baby is born.
The final phase of birth is the postpartum phase. It begins when the baby is born and ends when the placenta is expelled. After the baby is born, the uterus initially relaxes before contractions begin again about 15 minutes afterward. This last phase of birth is the shortest phase, lasting 10 to 20 minutes. The duration of each phase may depend, among other things, on whether or not it is the first birth.
But always remember, that each birth can proceed at a different pace. Don’t drive yourself crazy in advance! You will do great!
The time after birth
Puerperium with baby blues: what to watch out for after birth?
The period from six to eight weeks after birth is called the puerperium period. This period is particularly important because mother and child need to recover from the birth. In addition, this time is characterized by intensive getting to know each other and finding each other between parents and child. Before you go home with your baby, you spend a few more days in the hospital, depending on the type of birth. With a natural birth, the hospital stay is usually between 2 to 3 days, while with a cesarean section you have about four days of hospital stay. In an outpatient birth, you leave the clinic or birth center just a few hours after the baby is born.
At home, in familiar surroundings, many new experiences await and the new parents have time to get used to the new everyday life with baby. Especially for the moms, the time after the birth can be very intense. 80% of women, for example, experience the so-called baby blues. Despite the joy of having a baby, many moms feel like crying and have to deal with severe mood swings. This is due to hormonal changes after the birth. After all, not only does the body start to change again after the birth, but the hormones also get mixed up again. While estrogen and progesterone decrease, prolactin levels increase to stimulate milk production. But don’t worry, the hormone level settles down again and the emotional fluctuations disappear after a few days.

Important: Don’t take on too much during this time and concentrate on your child and your body. The birth demands a lot of strength, which is why you should use the time afterwards to recover. So take it slowly, give yourself breaks and don’t be afraid to ask for help.
Midwife aftercare: Who is my postpartum contact?
After the birth, many new things come up for parents and child, so it is quite normal if many questions arise during this time and you want a contact person. In the course of aftercare, midwives offer professional care and support after the birth. The midwife monitors wound healing and involution in the mother and also checks the growth and weight of the child. She also answers parents’ questions about the newborn, the new situation and can also provide assistance with breastfeeding. Midwives are there to support parents and can also offer encouragement and encouragement, especially after the first birth, to give parents peace of mind. In the first 10 days after the birth, midwives can even come daily for aftercare, after which two visits per week are still possible until the twelfth week.
Regression: When should I start regression?
Your body begins to regress all by itself, even in the first few days after birth. This is because there are often afterpains. These are contractions of the uterus, which slowly contracts again to reach its normal size. Regression can be somewhat faster in breastfeeding mothers, as the contraction of the uterus is supported by the breastfeeding hormone oxytocin. Regression also includes the healing of all internal and external wounds, as well as the wound from a cesarean section. If you want to support the process of involution and your overstretched muscles in the abdomen and legs with special involution gymnastics, you should keep a few things in mind. First of all, it is important that you do not start too early and that you consciously take the time of the postpartum period to recover and heal. Especially in the case of a cesarean section or perineal tear, you should wait until the stitches have healed. If the wounds and health are okay according to the postpartum midwife, light exercises can be started. For example, the pelvic floor muscles can be exercised, or when standing up, one leg can be placed after the other to challenge the lateral abdominal muscles. Regression takes about nine months, which is the same length of time as pregnancy. So don’t put yourself under pressure and give your body enough time.

Important: The same applies to the registration for a postnatal course as for a childbirth preparation course: as soon as possible! So you better take care of it early and secure a free place if you know that you want to attend a course.
Placenta: What can I do with the placenta after birth?
The placenta supplies the baby with oxygen and nutrients for over nine months and is the most important interface between mother and child. It is therefore understandable that some new mothers find it difficult to have the placenta disposed of by the hospital. After birth, the placenta is only examined by a midwife to ensure that it has been completely detached during the postpartum period, after which the woman can decide what to do with it. One option, for example, is to bury the placenta in the garden and plant a tree on it for the newborn. Recently, some women also have globules made for their child from their placenta or make them themselves. For this purpose, the placenta is first boiled and dried, and then processed into powder. Sometimes one also hears that the placenta can be eaten. This is supposed to prevent postpartum depression, relieve pain and promote involution, for example. However, these effects have not been scientifically proven.
Special features of a birth during a pandemic
Giving birth during a pandemic can have some unique aspects. Mama Christina gave birth to her son during the Corona pandemic and tells us about her experience.
The first difference to a birth under normal circumstances is that a mask has to be worn. However, the welfare of the pregnant woman still comes first. Therefore, the mask may usually be removed when the birth is relatively advanced, as it allows for better breathing. In addition, pregnant women must be tested upon arrival at the hospital. In Mama Christina’s case, this was after the first cervical check. If corona is suspected or present, the birth must take place unaccompanied. There is a special area, or delivery room, for these cases. However, if the test is negative, the birth can continue relatively normally. When the birth starts and the cervix opens, the partner is then allowed into the delivery room to support the expectant mom. Even after the birth, the partner is allowed to stay in the delivery room with the mother and baby for a few hours until they have to go to the maternity ward. If the baby needs to go to the neonatal unit after birth, the fresh parents can visit at any time to be there for their child.
An alternative in the pandemic can be, for example, an outpatient birth. However, this must be clarified with midwives and doctors. The prerequisite here is that mother and child feel well and there are no risks during the birth or illnesses. Being back in a familiar and safe environment immediately after the birth can be a wonderful experience for new moms and, of course, also for the partner. It is important that aftercare for mother and child is still provided, for example by an aftercare midwife.
Mama Christina’s comparison to giving birth under normal conditions:

“The fear of having to go through the birth alone and being alone in labor for a long time is very worrying before that. But this time I actually ‘enjoyed’ the ban on visits, I have to say. Intensive time to get to know each other as a couple and the full time to rest, without visits, I found really nice this time.”
You can do it!
Whether under normal conditions or during a pandemic, a birth is always an extraordinary experience that is associated with excitement. But you don’t have to be afraid, because you don’t have to go through this experience alone and you will be cared for and accompanied by competent clinic staff and your midwife. The main thing is that you feel comfortable and trust in your strength. It will all be worth it in the end when you can finally hold your little miracle in your arms!










Comments (0)